What is joint damage?
 Most joints in the body are synovial joints with articular cartilage moving on smooth articular cartilage.
Most joints in the body are synovial joints with articular cartilage moving on smooth articular cartilage.
The surface of the joint can become damaged for several reasons. The result can be a painful joint that limits your ability to do the things you love and your ability to work.
We are understanding more about joint wear and tear as time goes on. We know that damage to supportive structures such as the knee joint menisci has a bad effect on the joint, causing increased contact pressures and increasing the rate of wear. Joints that are not well aligned or that are unstable wear out more quickly; joints which have excess load put through them will also deteriorate more quickly.
Surgery often has a role to play in managing these aspects of joint damage.
We understand that factors in the knee contribute to healing and repair processes and other factors promote inflammation and damage in the joint
But what if…
- You have tried physiotherapy?
- Your joints are well aligned?
- There isn’t any unstable tissue in the joint?
- Your joint is stable?
- You have made efforts to keep at a healthy weight and reduce the impact on the joints in your daily activities?
For many patients in this situation, who want to delay or avoid surgery the answer could well be orthobiologics – biological treatments designed to improve the biological environment in the joint and support the cartilage.
What options do I have to treat joint wear and tear if I don’t want surgery?
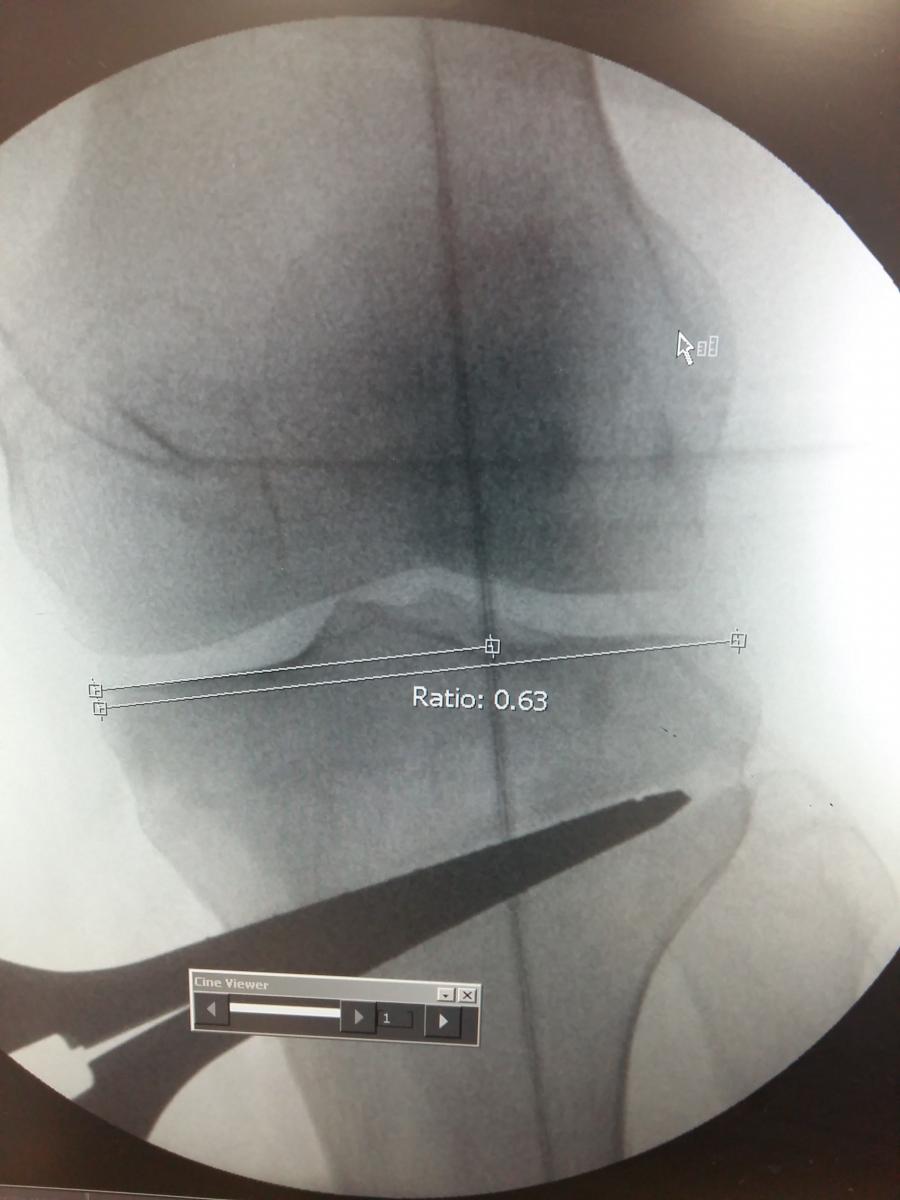
.jpg) There are numerous options to treat early to moderate joint wear and tear. With regard to orthobiologics, the results are generally less good with more advanced stages of joint wear and tear, although the benefits can still be worthwhile. If your degeneration is mild to moderate you are a good candidate to consider these treatments. If your joint is badly damaged and worn it may be more appropriate to consider other options
There are numerous options to treat early to moderate joint wear and tear. With regard to orthobiologics, the results are generally less good with more advanced stages of joint wear and tear, although the benefits can still be worthwhile. If your degeneration is mild to moderate you are a good candidate to consider these treatments. If your joint is badly damaged and worn it may be more appropriate to consider other options
You should discuss all the options open to you with your specialist/GP to ensure you are giving yourself the best chance of improving your pain and function.
At Midland Knee Protect Clinic we use the following treatments:
Autologous Conditioned Plasma (ACP) or Platelet Rich Plasma (PRP)
Other ways you can improve your symptoms
Obviously, not all knees (or indeed other joints) with wear and tear need surgery. In the early stages, there are several things that can be done to slow the progress of the condition and possibly even lead to a degree of recovery.
Weight control and Physiotherapy
A study in the British Medical Journal (Jenkinson, August 2009) confirmed that "A home based, self managed programme of simple knee strengthening exercises over a two year period can significantly reduce knee pain and improve knee function in overweight … people with knee pain. A moderate sustained weight loss is achievable with dietary intervention…". This means that, often with the help of a dietician, it is possible to maintain weight loss and that this has a significant effect on knee pain and function in the majority of cases.
Physiotherapy focuses on maintaining range of motion in the stiffening knee, regaining the loss of muscle power and stamina and improving normal walking patterns.
Whilst it is clear that doing exercise to lose weight will be very hard when knee pain restricts that exercise, it is important to remember that reducing calorie intake is even more important in this situation. If you cannot burn the energy off because the knee is too painful to exercise then it is imperative to reduce the energy being taken on board. This means reducing portion size and the quantity of high energy foods.
Steroid (corticosteroid)
Anti-inflammatory steroid injections do have a role in the temporary reduction of pain in joints with wear and tear inflammation. They are injected directly into the joint with care to avoid infection. Cortisone is a type of steroid that is produced naturally by a gland in your body called the adrenal gland. Cortisone is released from the adrenal gland when your body is under stress. They work by reducing the inflammatory process within the tissue/joint.
Side effects are uncommon but can include knee pain or 'cortisone flare,' a condition where the injected cortisone crystallizes and can cause a brief period of pain worse than before the injection. This usually lasts a day or two and is best treated by icing the injected area. Another common side-effect is whitening of the skin where the injection is given. This is only a concern in people with darker skin, and is not harmful, but patients should be aware of this. The most concerning risk is infection, especially if the injection is given into a joint. However, this is rare, particularly when carefully administered.
Physiotherapy
These highly trained practitioners can help significantly with maintaining range of motion and stability in joints and optimising the stamina and power of the surrounding muscles. Whether this therapy is to try to cope without surgery or in preparation for it, the benefits are significant.
Exercise
Maintaining general health with cardiovascular exercise is important for everyone but many surgeons are concerned about the potential damage that could be caused by this to the joints - particularly of the knee, hip and ankle.
Running:
The overall health benefits of cardiovascular exercise, such as running, are clear. It is also clear, that in certain circumstances, running can lead to overload injuries of muscles, tendons, and bone. It has not been established that running leads to degeneration of articular cartilage (osteoarthritis).
However, it is important to understand that runners with abnormal anatomy and those with significant previous injury are at increased risk for the development and progression of hip, knee and ankle osteoarthritis. It is also likely that athletes exposing themselves to very high levels of training (e.g. marathon runners) are also exposing themselves to a high risk of injury (up to 55% 1-year prevalence in one study - van Middelkoop 2008).
Resistance Training/gym work
In people with knee osteoarthritis pain, knee function, and knee performance (including maximum walking speed, time to stand from a chair, and balance) improve significantly following resistance training. This should initially be carried out in association with a physiotherapist.
Low joint impact sports
Many surgeons recommend such sports as low impact cycling, walking and swimming for patients with lower limb arthritis. This is because of the way the cartilage is loaded with these sports. These activities allow the cartilage lining of the joint to work without the impact loading of other activities. Current research suggests that this allows the fluid within the cartilage to function in a certain way: the joint glides with lower friction on a liquid surface that is "boosted" by some of the water being slightly absorbed by the porous cartilage. This leaves the "cartilage matrix" briefly in a higher concentration that provides better lubrication and shock absorbency. Also, when loaded gradually, the fluid in the knee works as a "fluid film lubricant" that provides hydrodynamic lubrication.
Medication
Numerous medications have been developed to reduce pain and many of these are developed specifically for people with arthritis.
These include:-
- Paracetamol
- Opioids (and opiates) such as tramadol and codeine
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) such as voltarol
- Analgesics directed at nerve pain reduction such as gabapentin
- Local anaesthetics such as lignocaine
- Glucosamine and Chondroitin
The best way to address pain control requirements is in close association with your surgeon and GP, gradually "going higher up the analgesic ladder" to stronger medications until control of pain symptoms is achieved. This should be in conjunction with the above recommendations.